Cognitive Assesment Guidelines
US Preventive Services Task Force guidelines—20201
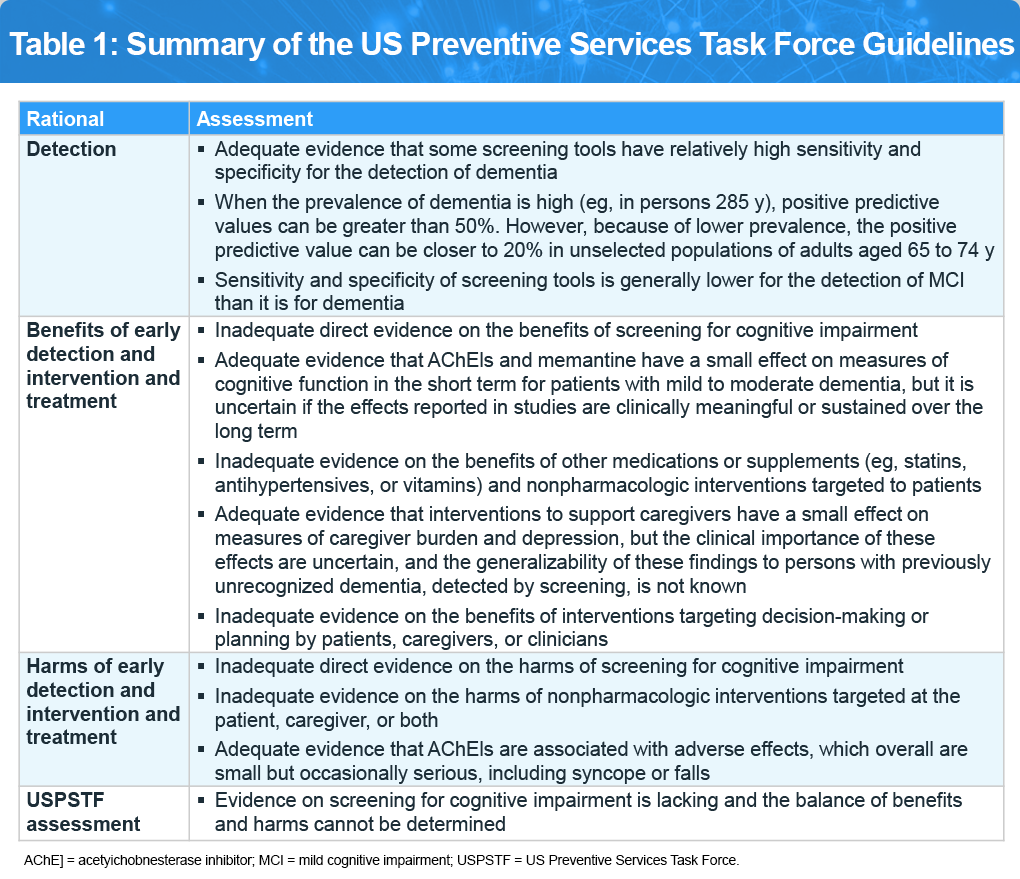
In its 2020 review on routine cognitive screening for adults aged 65 and older, the US Preventive Services Task Force concluded that there isn’t enough evidence to support or oppose routine screening. However, it emphasized the potential value of early detection. Clinicians are encouraged to stay vigilant for early indicators of cognitive decline—such as difficulties with memory or language—and to conduct further evaluation when warranted. Per the US Preventive Services Task Force, “this recommendation applies to community-dwelling older adults 65 years or older, without recognized signs or symptoms of cognitive impairment. Early detection and diagnosis of dementia through the assessment of signs and symptoms recognized by the patient, family, or clinician, which may be subtle, are not considered screening and are therefore not the focus of this recommendation.” Refer to Table 1 for additional details.
Alzheimer’s Association Guidelines2
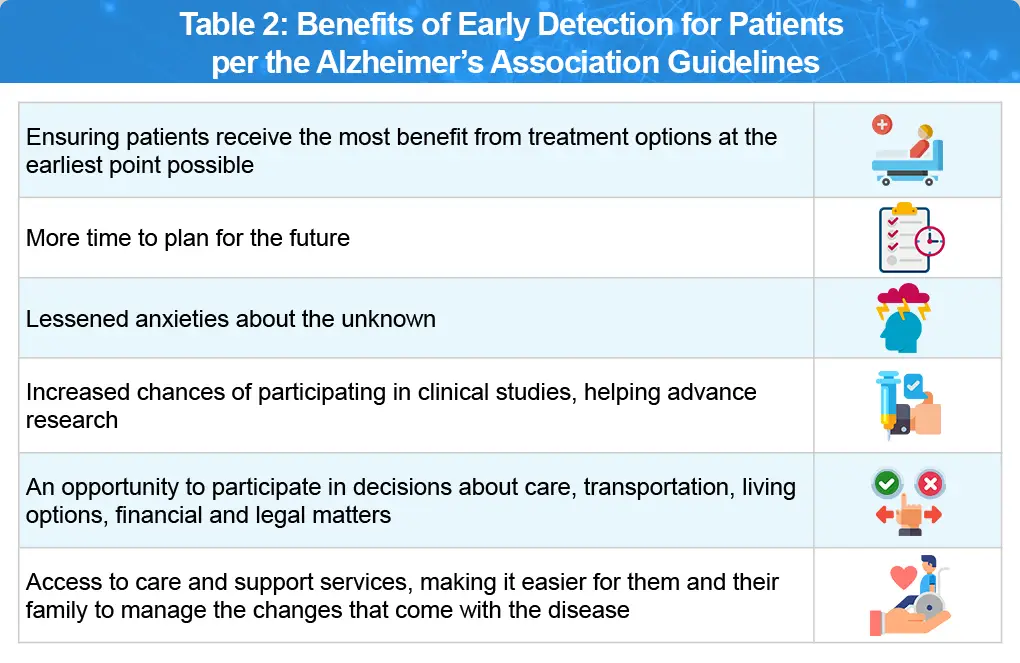
Per the Alzheimer’s Association the following population should be evaluated for cognitive impairment to benefit from early detection (Table 2):
- Individuals with memory concerns or other cognitive complaints
- Non-memory triggers listed are personality change, depression, deterioration of chronic disease without explanation, and falls or balance issues
- Informant reports of cognitive impairment, with or without patient concurrence
- Medicare beneficiaries, as part of the Annual Wellness Visit
American Academy of Family Physicians3
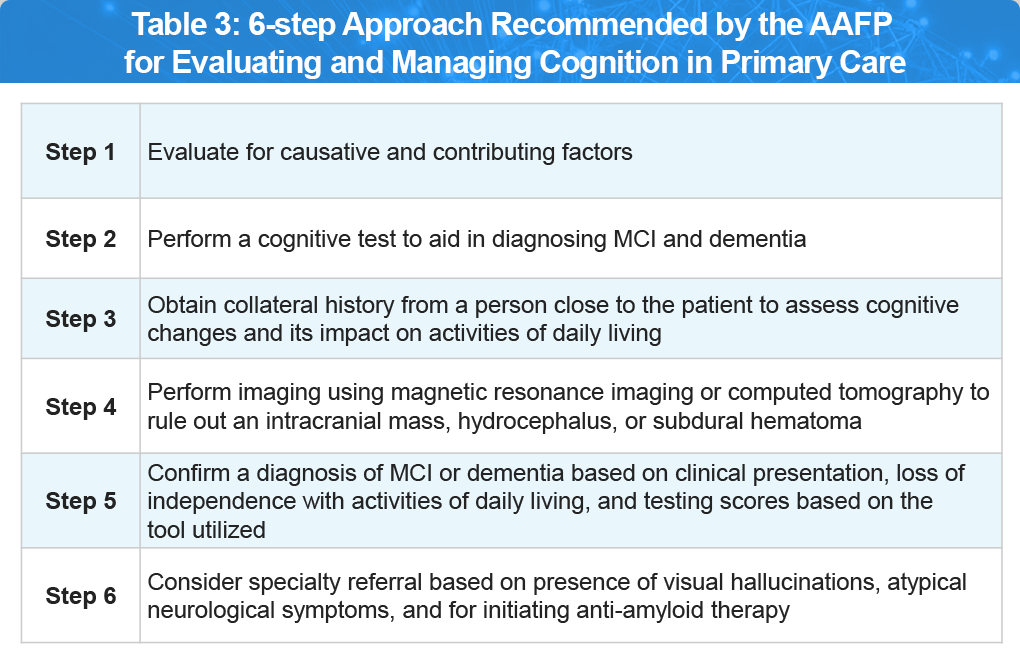
The AAFP guidelines recommend that an evaluation is best to be performed during a dedicated patient visit, accompanied by a family member or close friend. Per the guidelines, clinicians should recognize the warning signs of cognitive impairment, treat contributing factors, diagnose MCI and dementia and help manage these conditions as they progress in a stepwise manner (Table 3).
During follow-up visits, clinicians can discuss brain health and safety, provide advance directives, and refer patients and caregivers to helpful resources such as:
Suggested Workflow/Algorithm4
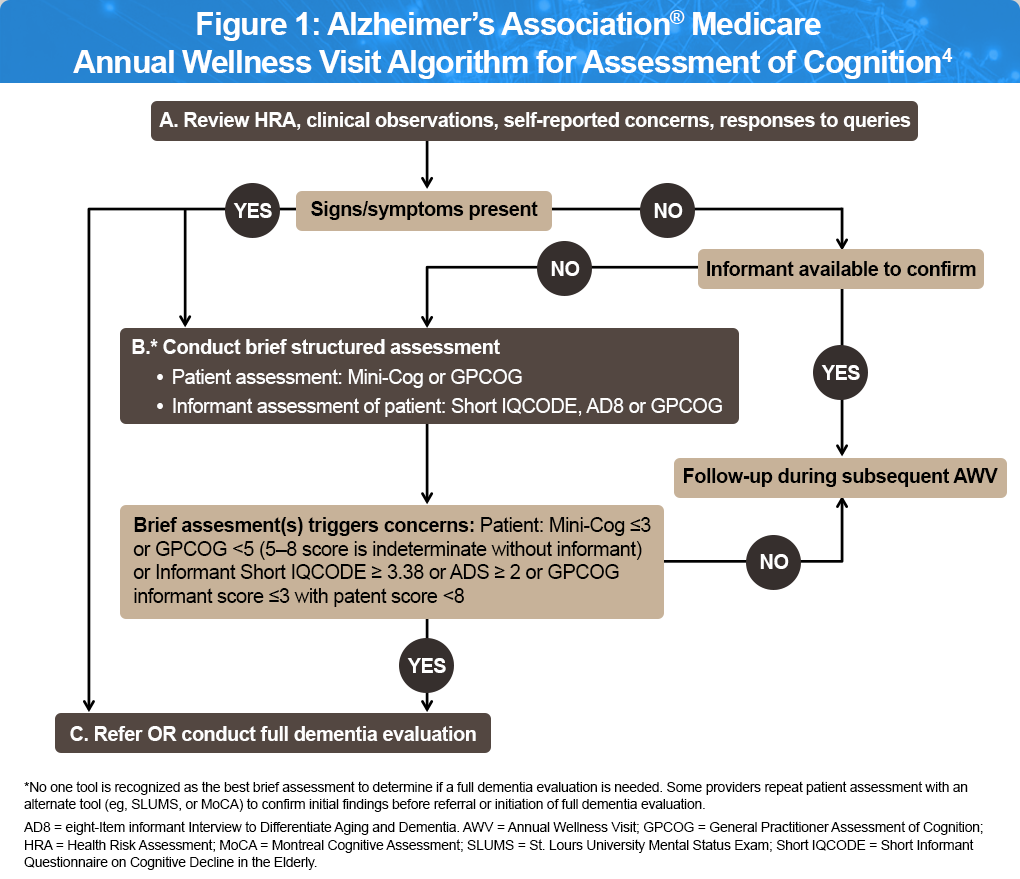
The Alzheimer’s Association convened a panel of experienced clinicians to develop practical, efficient, and straightforward guidelines for identifying cognitive impairment in primary care. The resulting algorithm (Figure 1) includes patient history, clinical observations, and input from the patient, family, or caregivers. Recognizing that cognitive assessment tools can enhance dementia detection in primary care, the group recommended several brief screening instruments—all of which can be completed in five minutes or less by a doctor or trained staff.
Summary
Primary care plays a key role in early cognitive assessment, brain health discussions, and addressing reversible causes of decline, making it essential for detecting cognitive impairment early. Early detection can slow the progression of MCI and related dementias, improve quality of life, and reduce associated risks and disparities. Integrating early testing per recommended guidelines and resources into routine care is crucial to fully realize these benefits for patients and their families.
References
- U.S. Preventive Services Task Force. Cognitive Impairment in Older Adults: Screening (https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cognitive-impairment-in-older-adults-screening).
- Alzheimer’s Association. Cognitive Screening and Assessment (https://www.alz.org/professionals/health-systems-medical-professionals/cognitive-assessment).
- U.S. Preventive Services Task Force. Screening for Cognitive Impairment in Older Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323(8):757–763.
- Cordell CB, Borson S, Boustani M, et al. Alzheimer’sAssociation recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
All URLs accessed on September 22, 2025.