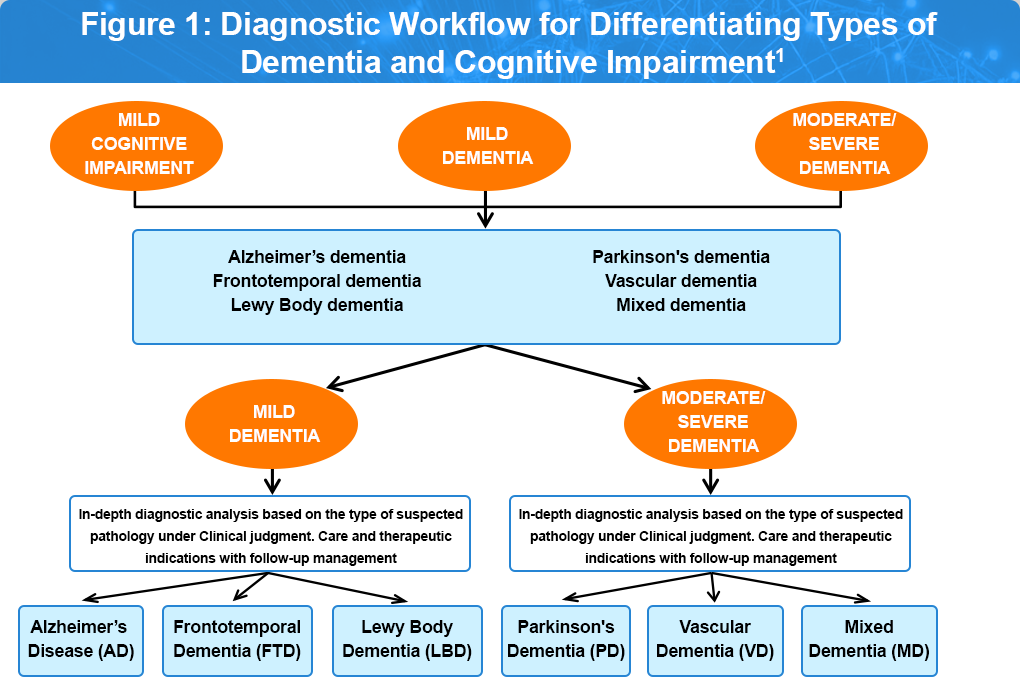
Differential Diagnoses
Not all cognitive changes are due to Alzheimer’s disease or related dementias. During the diagnostic work-up for memory loss, confusion, or other cognitive symptoms, it is critical to consider a broad differential diagnosis. Identifying the correct underlying cause enables appropriate treatment, avoids misdiagnosis, and improves patient outcomes. Figure 1 highlights the progressive diseases that cause gradual cognitive decline and the diagnostic workflow for differentiating among these conditions.1
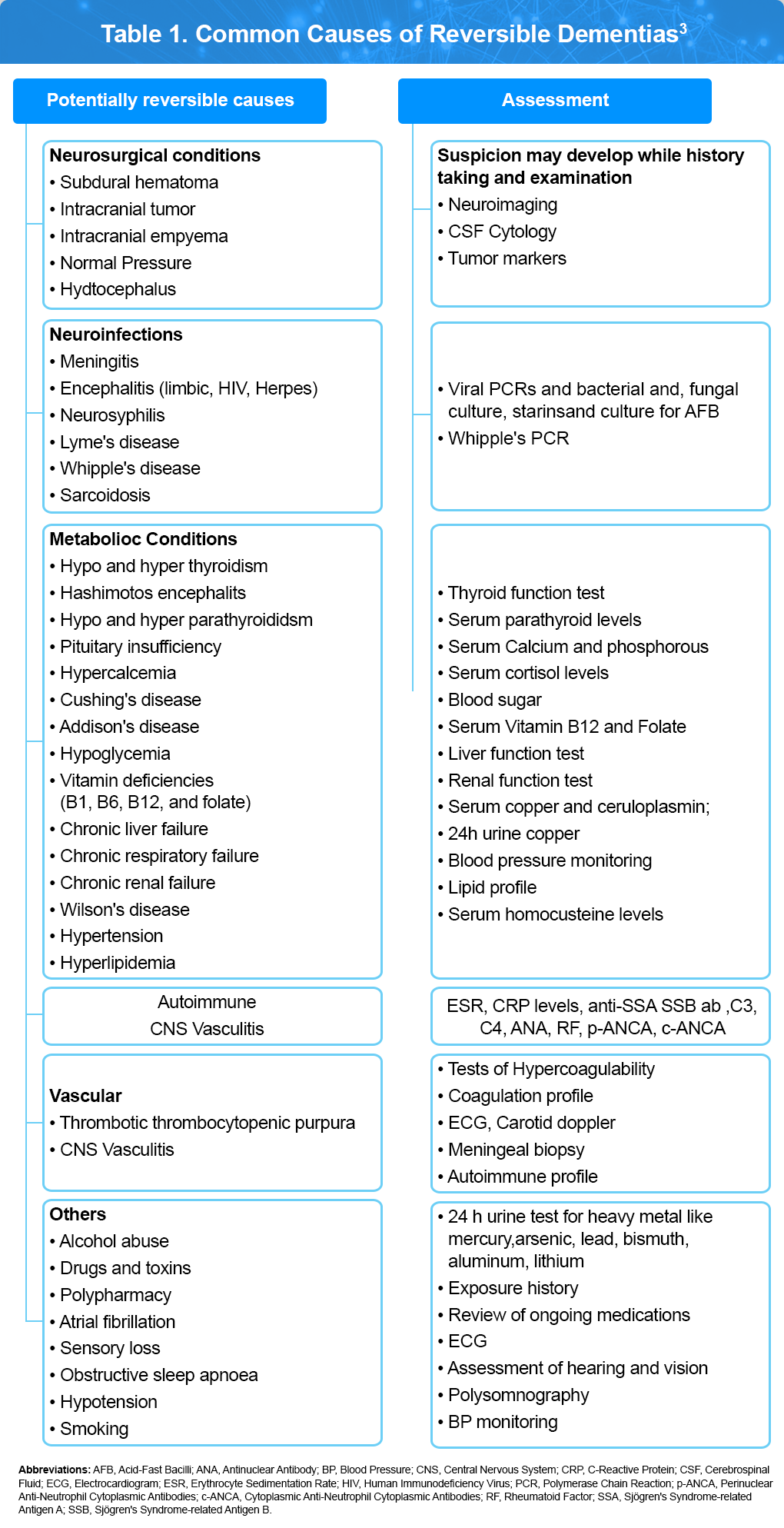
Additionally, it is Important to rule out potential reversible causes of cognitive decline. Reversible dementias refer to conditions that cause cognitive or behavioral symptoms, which may improve or fully resolve when the underlying cause is properly treated. Numerous potential factors have been identified that can lead to temporary neurocognitive impairment in older adults (see Table 1). However, the term “reversible dementia” can be misleading, as many metabolic causes that affect cognition also share features with delirium, leading to diagnostic overlap.2
Summary
Diagnosing cognitive impairment requires a broad differential diagnosis and careful consideration of clinical signs, biomarkers, and imaging findings. While Alzheimer’s disease is common, many other conditions can mimic or contribute to cognitive decline. A structured, evidence-based approach allows clinicians to provide timely and accurate diagnoses, improving care and outcomes for patients and families.
References
- Gareri P, Cotroneo AM, Gelmini G, Mossello E, Massaia M; Touch Working Group. An algorithm for the early diagnosis and correct approach to dementia management: results of a multiprofessional team. Aging Clin Exp Res. 2024;36:102.
- Chari D, Ali R, Gupta R. Reversible dementia in elderly: Really uncommon?. J Geriatr Mental Health 2015;2:30-37.
- Subramanyam AA, Singh S, Raut NB. Clinical practice guidelines for assessment and management of mild neurocognitive disorder. Indian J Psychiatry. 2025 Jan;67:21-40. Erratum in: Indian J Psychiatry. 2025;67:280.
Accessed on September 22, 2025.